In a broken mental health system, a tiny jail cell becomes an institution of last resort
Polson, Montana — When someone accused of a crime in this small northwestern Montana town needs mental health care, chances are they’ll be locked in a basement jail cell the size of a walk-in closet.
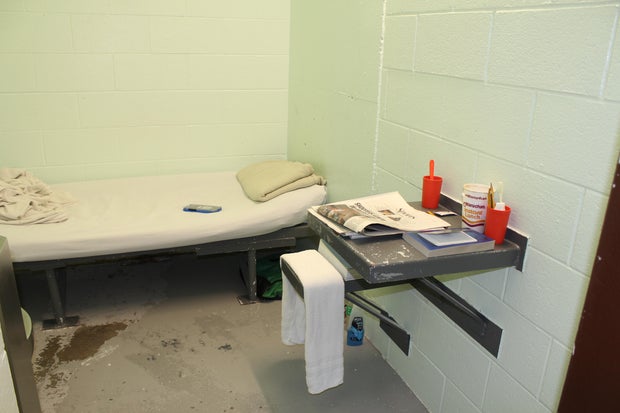
Prisoners, some held in this isolation cell for months, have scratched initials and the phrase “love hurts” into the metal door’s brown paint. Their pacing has worn a path into the cement floor. Many are held in a sort of limbo, not convicted of a crime but not stable enough to be released. They sleep on a narrow cot next to a toilet. The only view is a fluorescent-lit hallway visible through a small window in the door.
Lake County Attorney James Lapotka stood at the cell’s center talking about the people he helps confine here. He stretched out his arms, his fingertips just shy of touching opposite walls. “I’m getting anxiety just being in here,” Lapotka said.
Katheryn Houghton / KFF Health News
Last year, a man sentenced for stealing a rifle stayed in that cell 129 days. He was waiting for a spot to open at Montana’s only state-run psychiatric hospital after a mental health evaluator deemed he needed care, according to court records.
A man in the next cell around the same time was on the same waitlist roughly five months. He faced near-daily stints in the jail’s emergency restraint chair — a steel contraption wrapped in foam with straps for his shoulders, arms, and legs. He regularly saw the jail’s mental health doctor. Still, Joel Shearer, a Lake County detention commander, said the man routinely experienced psychotic episodes and asked to be locked in the chair when he felt one coming on and stayed there until his screams subsided.
“Somebody who’s having a mental health crisis — they don’t belong here,” Lapotka said. “We don’t have anywhere else.”
Katheryn Houghton / KFF Health News
Lake County’s two, roughly 30-square-foot isolation cells are an example of how communities nationwide are failing to provide mental health services — crisis care, in particular. Nearly half of the people locked in local jails in the U.S. have a mental illness.
More than half of Wyoming’s 23 sheriffs told lawmakers there that they were housing people in crisis awaiting mental health care for months, WyoFile reported in January. Nevada has struggled despite a $500 daily fine for each jailed patient whose treatment is delayed. Disability Rights Oregon has said delays in that state continue after two people died in jail while on the state’s psychiatric waitlist.
In Montana, counties are jailing mental health patients they’re not equipped to handle when the Montana State Hospital is at capacity. Few local hospitals have their own inpatient psychiatric beds. As a result, people arrested for anything from petty theft to felony assault can be jailed for months or longer as their mental health worsens. Many haven’t been convicted of a crime.
Montana officials have known for years they have a problem. State officials have said they don’t have space for all the people ordered to the hospital. The psychiatric hospital has 270 beds, with 54 for people in the criminal justice system. Staffing shortages can shrink that capacity further.
The Montana Department of Public Health and Human Services backed two bills this legislative session that would shield the state from liability for delays when the Montana State Hospital is full. Ahead of the bills, the agency wrote the hospital has “struggled to maintain appropriate levels of care” due to money and staffing constraints, a lack of community-based services, and having no control over the flow patients Montana courts send its way.
The agency also announced April 23 that $6.5 million was available through one-time grants to help set up jail-based mental health stabilization services.
Officials have said patients deserve care closer to home, in less restrictive settings. But counties say the local services needed don’t exist.
“You have to do the hard things first,” said Matt Kuntz, executive director of the Montana chapter of the National Alliance on Mental Illness. “You have to build the beds.”
Health advocates have backed a proposal that would require the state to pay for community commitments. That measure is headed to Republican Gov. Greg Gianforte after passing the state House and Senate. Another bill that was still pending would create a new psychiatric hospital for people in the justice system. But implementing those ideas could take years.
The number of inpatient beds for people with a serious mental illness nationwide has plummeted. At one time, that drop was intentional, part of a movement away from locking people up in state-run mental hospitals. But the intended fix, local homelike centers, hasn’t filled the void.
One of Montana’s biggest providers, Western Montana Mental Health Center, had to close some of its crisis sites because of money problems, said Western’s CEO, Bob Lopp. That includes a facility less than a mile from the Lake County jail.
“If that’s not where the funding is, you can’t just do it for the sake of argument and hope that it comes,” Lopp said.
Gianforte has promised to pour money into rebuilding the state’s behavioral health system. Mental health workers in small towns find such promises hard to trust after seeing local services come and go for years.
Health department spokesperson Holly Matkin said the agency is proud of its work to fix “systems that have been broken for too long” and that it will improve services for people who need inpatient care in their communities.
Lake County is known to outsiders as an Instagram-worthy stop on their way to Glacier National Park. It overlaps with the Flathead Indian Reservation, land of the Bitterroot Salish, Upper Pend d’Oreille, and Kootenai tribes. It’s home to a slice of the Rocky Mountains and a gateway to millions of acres of wilderness. Polson, the county seat and site of the jail, is a town of 5,600 on the southern shore of Flathead Lake, one of the largest lakes west of the Mississippi River.
Vincent River has worked as the jail’s sole mental health clinician for 25 years. He said he’s not always available because he’s the only psychologist in four northwestern Montana counties evaluating whether a person in jail needs psychiatric care.
Some are released without care if they linger too long on the state hospital’s waitlist.
“I talk to these family members. I hear them plead with me with their fear in their voices and tell me all that’s been going on for days or weeks or months,” River said. “And then I can’t get people into the hospital. That is a giant crisis.”
It’s not just the state hospital. River said he can’t get people into any psychiatric bed in Montana because there are too few. Instead, he tries to stabilize people while they’re jailed. That has shortfalls.
The jail can’t force someone in psychosis to take medication without a court order and a qualified doctor on hand to administer the prescription. Lake County’s aging facility has faced lawsuits because of poor conditions amid overcrowding, and River has to see patients wherever there’s room.
There isn’t even space for the jail’s restraint chair. Jail workers leave strapped-down prisoners in a hallway or locker room.
River said many gradually get better and leave isolation. Some don’t.
“They languish there, psychotic and lonely,” he said, “at the mercy of what the voices are telling them.”
Locals are working to fill some gaps. A mobile team launched in February is staffed by people who have lived with mental and substance use disorders to provide peer support. But someone truly in crisis has only two options: jail or an emergency room.
The room reserved for people in crisis at Providence St. Joseph Medical Center in Polson leaves patients both isolated and without privacy. The locked door’s thick glass looks onto a busy emergency room hallway.
Those who deteriorate enough to be deemed dangerous to themselves or others are sent down the road to jail.
Rebecca Bontadelli, an ER physician, said patients can be housed in the room for days as hospital staffers scour Montana and nearby states for an open psychiatric bed. Some reject care in the meantime.
“We’re not really helping them,” Bontadelli said. “They feel like they’re in prison.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.